Description
Baxter 2B0864 - SOLTUION, ISOTONIC GENTAMICN SULFAT INJ 1, 24/CS
Gentamicin Sulfate in 0.9% Sodium Chloride Injection, 120 mg in 100 mL VIAFLEX Plus Container
Boxed Warning
WARNINGS
Patients treated with aminoglycosides should be under close clinical observation because of the potential toxicity associated with their use. As with other aminoglycosides, gentamicin sulfate is potentially nephrotoxic. The risk of nephrotoxicity is greater in patients with impaired renal function and in those who receive high dosage or prolonged therapy.
Neurotoxicity manifested by ototoxicity, both vestibular and auditory, can occur in patients treated with gentamicin sulfate, primarily those with pre-existing renal damage and in patients with normal renal function treated with higher doses and/or for longer periods than recommended. Aminoglycoside-induced ototoxicity is usually irreversible. Other manifestations of neurotoxicity may include numbness, skin tingling, muscle twitching and convulsions.
Renal and eighth cranial nerve function should be closely monitored, especially in patients with known or suspected reduced renal function at onset of therapy and also in those whose renal function is initially normal but who develop signs of renal dysfunction during therapy. Urine should be examined for decreased specific gravity, increased excretion of protein, and the presence of cells or casts. Blood urea nitrogen (BUN), serum creatinine, or creatinine clearance should be determined periodically. When feasible, it is recommended that serial audiograms be obtained in patients old enough to be tested, particularly high-risk patients. Evidence of ototoxicity (dizziness, vertigo, tinnitus, roaring in the ears or hearing loss) or nephrotoxicity requires dosage adjustment or discontinuance of the drug. As with the other aminoglycosides, on rare occasions changes in renal and eighth cranial nerve function may not become manifest until soon after completion of therapy.
Serum concentrations of aminoglycosides should be monitored when feasible to assure adequate levels and to avoid potentially toxic levels. When monitoring gentamicin peak concentrations, dosage should be adjusted so that prolonged levels above 12 mcg/mL are avoided. When monitoring gentamicin trough concentrations, dosage should be adjusted so that levels above 2 mcg/mL are avoided. Excessive peak and/or trough serum concentrations of aminoglycosides may increase the risk of renal and eighth cranial nerve toxicity. In the event of overdose or toxic reactions, hemodialysis may aid in the removal of gentamicin from the blood, especially if renal function is, or becomes compromised. The rate of removal of gentamicin is considerably lower by peritoneal dialysis than it is by hemodialysis.
Concurrent and/or sequential systemic or topical use of other potentially neurotoxic and/or nephrotoxic drugs, such as cisplatin, cephaloridine, kanamycin, amikacin, neomycin, polymyxin B, colistin, paromomycin, streptomycin, tobramycin, vancomycin, and viomycin, should be avoided (see PRECAUTIONS, DRUG INTERACTIONS section).
Other factors which may increase patient risk of toxicity are advanced age and dehydration (see PRECAUTIONS, GERIATRIC USE and DOSAGE AND ADMINISTRATION sections).
The concurrent use of gentamicin with potent diuretics, such as ethacrynic acid or furosemide, should be avoided, since certain diuretics by themselves may cause ototoxicity. In addition, when administered intravenously, diuretics may enhance aminoglycoside toxicity by altering the antibiotic concentration in serum and tissue (see PRECAUTIONS, DRUG INTERACTIONS section).
Aminoglycosides can cause fetal harm when administered to a pregnant woman (see WARNINGS and PRECAUTIONS, PREGNANCY sections).
Gentamicin Sulfate in Sodium Chloride
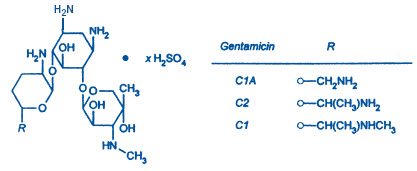
Gentamicin Sulfate, USP, a water soluble antibiotic of the aminoglycoside group, is derived from Micromonospora purpurea, and actinomycete.
Gentamicin Sulfate in 0.9% Sodium Chloride Injection is a sterile, nonpyrogenic solution of Gentamicin Sulfate, USP in water for injection with 9 mg/mL sodium chloride (NaCl) to provide isotonicity. The solution is intended for intravenous use and requires no further dilution. pH may be adjusted with sulfuric acid or sodium hydroxide and is approximately 4.5.
VIAFLEX Plus Container
This VIAFLEX Plus plastic container is fabricated from a specially formulated polyvinyl chloride (PL 146 Plastic). VIAFLEX Plus on the container indicates the presence of a drug additive in a drug vehicle. The VIAFLEX Plus plastic container system utilizes the same container as the VIAFLEX plastic container system. The amount of water that can permeate from inside the container into the overwrap is insufficient to affect the solution significantly. Solutions in contact with the plastic container can leach out certain of its chemical components in very small amounts within the expiration period, e.g., di-2-ethylhexyl phthalate (DEHP), up to 5 parts per million. However, the safety of the plastic has been confirmed in tests in animals according to USP biological tests for plastic containers as well as by tissue culture toxicity studies.
Clinical Pharmacology
After intramuscular (IM) administration of gentamicin sulfate, peak serum concentrations usually occur between 30 to 60 minutes and serum levels are measurable for 6 to 8 hours. When gentamicin is administered by intravenous (IV) infusion over a two-hour period, the serum concentrations are similar to those obtained by intramuscular administration.
In patients with normal renal function, peak serum concentrations of gentamicin (mcg/mL) are usually up to four times the single intramuscular dose (mg/kg); for example, a 1 mg/kg injection in adults may be expected to result in a peak serum concentration up to 4 mcg/mL; a 1.5 mg/kg dose may produce levels up to 6 mcg/mL. While some variation is to be expected due to a number of variables such as age, body temperature, surface area and physiologic differences, the individual patient given the same dose tends to have similar levels in repeated determinations. Gentamicin administered at 1 mg/kg every eight hours for the usual 7- to 10-day treatment period to patients with normal renal function does not accumulate in the serum.
Gentamicin, like all aminoglycosides, may accumulate in the serum and tissue of patients treated with higher doses and/or for prolonged periods, particularly in the presence of impaired renal function. In adult patients, treatment with gentamicin dosages of 4 mg/kg/day or higher for seven to ten days may result in a slight, progressive rise in both peak and trough concentrations. In patients with impaired renal function, gentamicin is cleared from the body more slowly than in patients with normal renal function. The more severe the impairment, the slower the clearance. Dosage must be adjusted.
Since gentamicin is distributed in extracellular fluid, peak serum concentrations may be lower than usual in adult patients who have a large volume of this fluid. Serum concentrations of gentamicin in febrile patients may be lower than those in afebrile patients given the same dose. When body temperature returns to normal, serum concentrations of the drug may rise. Febrile and anemic states may be associated with a shorter than usual serum half-life. (Dosage adjustment is usually not necessary.) In severely burned patients, the half-life may be significantly decreased and resulting serum concentrations may be lower than anticipated from the mg/kg dose.
Protein binding studies have indicated that the degree of gentamicin binding is low. Depending upon the methods used for testing, this may be between 0 and 30%.
After initial administration to patients with normal renal function, generally 70% or more of the gentamicin dose is recoverable in the urine in 24 hours; concentrations in urine above 100 mcg/mL may be achieved. Little, if any, metabolic transformation occurs; the drug is excreted principally by glomerular filtration. After several days of treatment, the amount of gentamicin excreted in the urine approaches the daily dose administered. As with other aminoglycosides, a small amount of the gentamicin dose may be retained in the tissues, especially in the kidneys. Minute quantities of aminoglycosides have been detected in the urine weeks after the drug administration was discontinued. Renal clearance of gentamicin is similar to that of endogenous creatinine.
In patients with marked impairment of renal function, there is a decrease in the concentration of aminoglycosides in urine and in their penetration into defective renal parenchyma. This decreased drug excretion, together with the potential nephrotoxicity of aminoglycosides, should be considered when treating such patients who have urinary tract infections.
Probenecid does not affect renal tubular transport of gentamicin.
Indications and Usage
To reduce the development of drug-resistant bacteria and maintain the effectiveness of Gentamicin Sulfate in 0.9% Sodium Chloride Injection and other antibacterial drugs, Gentamicin Sulfate in 0.9% Sodium Chloride Injection should be used only to treat or prevent infections that are proven or strongly suspected to be caused by susceptible bacteria. When culture and susceptibility information are available, they should be considered in selecting or modifying antibacterial therapy. In the absence of such data, local epidemiology and susceptibility patterns may contribute to the empiric selection of therapy.
Gentamicin Sulfate in 0.9% Sodium Chloride Injection is indicated in the treatment of serious infections caused by susceptible strains of the following microorganisms: Pseudomonas aeruginosa, Proteus species (indole-positive and indole-negative), Escherichia coli, Klebsiella-Enterobacter- Serratia species, Citrobacter species, and Staphylococcus species (coagulase-positive and coagulase-negative).
Clinical studies have shown gentamicin sulfate to be effective in bacterial neonatal sepsis; bacterial septicemia; and serious bacterial infections of the central nervous system (meningitis), urinary tract, respiratory tract, gastrointestinal tract (including peritonitis), skin, bone and soft tissue (including burns). Aminoglycosides, including gentamicin, are not indicated in uncomplicated initial episodes of urinary tract infections unless the causative organisms are susceptible to these antibiotics and are not susceptible to antibiotics having less potential for toxicity.
Specimens for bacterial culture should be obtained to isolate and identify causative organisms and to determine their susceptibility to gentamicin.
Gentamicin Sulfate in 0.9% Sodium Chloride Injection may be considered as initial therapy in suspected or confirmed gram-negative infections, and therapy may be instituted before obtaining results of susceptibility testing. The decision to continue therapy with this drug should be based on the results of susceptibility tests, the severity of the infection, and the important additional concepts contained in the boxed WARNINGS. If the causative organisms are resistant to gentamicin, other appropriate therapy should be instituted.
In serious infections when the causative organisms are unknown, Gentamicin Sulfate in 0.9% Sodium Chloride Injection may be administered as initial therapy in conjunction with a penicillin-type or cephalosporin-type drug before obtaining results of susceptibility testing. If anaerobic organisms are suspected as etiologic agents, consideration should be given to using other suitable antimicrobial therapy in conjunction with gentamicin. Following identification of the organism and its susceptibility, appropriate antibiotic therapy should then be continued.
Gentamicin injection has been used effectively in combination with carbenicillin for the treatment of life-threatening infections caused by Pseudomonas aeruginosa. It has also been found effective when used in conjunction with a penicillin-type drug for the treatment of endocarditis caused by group D streptococci.
Gentamicin injection has also been shown to be effective in the treatment of serious staphylococcal infections. While not the antibiotic of first choice, gentamicin may be considered when penicillins or other less potentially toxic drugs are contraindicated and bacterial susceptibility tests and clinical judgement indicate its use. It may also be considered in mixed infections caused by susceptible strains of staphylococci and gram-negative organisms.
In the neonate with suspected bacterial sepsis or staphylococcal pneumonia, a penicillin-type drug is also usually indicated as concomitant therapy with gentamicin (see PRECAUTIONS, PEDIATRIC USE and DOSAGE AND ADMINISTRATION sections).
Contraindications
Hypersensitivity to gentamicin is a contraindication to its use. A history of hypersensitivity or serious toxic reactions to other aminoglycosides may contraindicate use of gentamicin because of known cross-sensitivity of patients to drugs in this class.
Warnings
Aminoglycosides can cause fetal harm when administered to a pregnant woman. Aminoglycoside antibiotics cross the placenta, and there have been several reports of total irreversible bilateral congenital deafness in children whose mothers received streptomycin during pregnancy. Serious side effects to mother, fetus or newborn have not been reported in the treatment of pregnant women with other aminoglycosides. Animal reproduction studies conducted on rats and rabbits did not reveal evidence of impaired fertility or harm to the fetus due to gentamicin sulfate. It is not known whether gentamicin sulfate can cause fetal harm when administered to a pregnant woman or can affect reproduction capacity. If gentamicin is used during pregnancy or if the patient becomes pregnant while taking gentamicin, she should be apprised of the potential hazard to the fetus.
Solutions containing sodium ions should be used with great care, if at all, in patients with congestive heart failure, severe renal insufficiency, and in clinical states in which there exists edema with sodium retention.
Precautions
General
Prescribing Gentamicin Sulfate in 0.9% Sodium Chloride Injection in the absence of a proven or strongly suspected bacterial infection or a prophylactic indication is unlikely to provide benefit to the patient and increases the risk of the development of drug-resistant bacteria.
Do not use additives or premix with other drugs. See DOSAGE AND ADMINISTRATION.
Neurotoxic and nephrotoxic antibiotics may be almost completely absorbed from body surfaces (except the urinary bladder) after local irrigation and after topical application during surgical procedures. The potential toxic effects of antibiotics administered in this fashion (neuromuscular blockade, respiratory paralysis, oto- and nephrotoxicity) should be considered (see boxed WARNINGS).
Aminoglycosides should be used with caution in patients with neuromuscular disorders such as myasthenia gravis or parkinsonism, since these drugs may aggravate muscle weakness because of their potential curare-like effects on the neuromuscular junction. During or following gentamicin therapy, paresthesias, tetany, positive Chvostek and Trousseau signs and mental confusion have been described in patients with hypomagnesemia, hypocalcemia and hypokalemia. When this has occurred in infants, tetany and muscle weakness has been described. Both adults and infants required appropriate corrective electrolyte therapy (see PRECAUTIONS, PEDIATRIC USE section).
A Fanconi-like syndrome, with aminoaciduria and metabolic acidosis has been reported in some adults and infants being given gentamicin injections.
Cross allergenicity among aminoglycosides has been demonstrated.
Patients should be well hydrated during treatment.
Treatment with gentamicin may result in overgrowth of nonsusceptible organisms. If this occurs, appropriate therapy is indicated.
See boxed WARNINGS regarding concurrent use of potent diuretics and regarding concurrent and/or sequential use of other neurotoxic and/or nephrotoxic antibiotics, and for other essential information (see also PRECAUTIONS, DRUG INTERACTIONS section).
Information for Patients
Patients should be counseled that antibacterial drugs including Gentamicin Sulfate in 0.9% Sodium Chloride Injection should only be used to treat bacterial infections. They do not treat viral infections (e.g., the common cold). When Gentamicin Sulfate in 0.9% Sodium Chloride Injection is prescribed to treat a bacterial infection, patients should be told that although it is common to feel better early in the course of therapy, the medication should be taken exactly as directed. Skipping doses or not completing the full course of therapy may (1) decrease the effectiveness of the immediate treatment and (2) increase the likelihood that bacteria will develop resistance and will not be treatable by Gentamicin Sulfate in 0.9% Sodium Chloride Injection or other antibacterial drugs in the future.
Laboratory Tests
Laboratory abnormalities possibly related to gentamicin include: increased levels of serum transaminase (SGOT, SGPT), serum LDH and billirubin; decreased serum calcium, magnesium, sodium and potassium; anemia, leukopenia, granulocytopenia, transient agranulocytosis, eosinophilia, increased and decreased reticulocyte counts and thrombocytopenia. While clinical laboratory test abnormalities may be isolated findings, they may also be associated with clinically related signs and symptoms. For example, tetany and muscle weakness may be associated with hypomagnesemia, hypocalcemia, and hypokalemia.
Drug Interactions
The concurrent use of gentamicin with potent diuretics, such as ethacrynic acid or furosemide, should be avoided, since certain diuretics by themselves may cause ototoxicity. In addition, when administered intravenously, diuretics may enhance aminoglycoside toxicity by altering the antibiotic concentration in serum and tissue.
Concurrent and/or sequential systemic or topical use of other potentially neurotoxic and/or nephrotoxic drugs such as cisplatin, cephaloridine, kanamycin, amikacin, neomycin, polymyxin B, colistin, paromomycin, streptomycin, tobramycin, vancomycin, and viomycin, should be avoided.
Increased nephrotoxicity has been reported following concomitant administration of aminoglycoside antibiotics and cephalosporins.
Neuromuscular blockade and respiratory paralysis have been reported in the cat receiving high doses (40 mg/kg) of gentamicin. The possibility of these phenomena occurring in man should be considered if aminoglycosides are administered by any route to patients receiving anesthetics, or to patients receiving neuro-muscular blocking agents, such as succinylcholine, tubocurarine, or decamethonium, or in patients receiving massive transfusions of citrate-anticoagulated blood. If neuromuscular blockade occurs, calcium salts may reverse it.
Although the in vitro mixing of gentamicin and carbenicillin results in a rapid and significant inactivation of gentamicin, this interaction has not been demonstrated in patients with normal renal function who received both drugs by different routes of administration. A reduction in gentamicin serum half-life has been reported in patients with severe renal impairment receiving carbenicillin concomitantly with gentamicin.
Probenecid does not affect renal tubular transport of gentamicin.
Pregnancy
Pregnancy Category D.
Aminoglycosides can cause fetal harm when administered to a pregnant woman. Aminoglycoside antibiotics cross the placenta and there have been several reports of total irreversible bilateral congenital deafness in children whose mothers received streptomycin during pregnancy. Serious side effects to mother, fetus, or newborn have not been reported in the treatment of pregnant women with other aminoglycosides. Animal reproduction studies conducted on rats and rabbits did not reveal evidence of impaired fertility or harm to the fetus due to gentamicin sulfate. It is not known whether gentamicin sulfate can cause fetal harm when administered to a pregnant woman or can affect reproduction capacity. If gentamicin is used during pregnancy or if the patient becomes pregnant while taking gentamicin, she should be apprised of the potential hazard to the fetus.
Nursing Mothers
It is not known whether this drug is excreted in human milk. Because many drugs are excreted in human milk and because of the potential for serious adverse reactions in nursing infants from gentamicin, a decision should be made whether to discontinue the drug, taking into account the importance of the drug to the mother.
Pediatric Use
In the neonate with suspected bacterial sepsis or staphylococcal pneumonia, a penicillin-type drug is also usually indicated as concomitant therapy with gentamicin.
During or following gentamicin therapy, paresthesias, tetany, positive Chvostek and Trousseau signs and mental confusion have been described in patients with hypomagnesemia, hypocalcemia and hypokalemia. When this has occurred in infants, tetany and muscle weakness have been described. Both adults and infants required appropriate corrective electrolyte therapy.
A Fanconi-like syndrome, with aminoaciduria and metabolic acidosis has been reported in some adults and infants being given gentamicin injections.
Geriatric Use
This drug is known to be substantially excreted by the kidney, and the risk of toxic reactions to this drug may be greater in patients with impaired renal function. Because elderly patients are more likely to have decreased renal function, care should be taken in dose selection, and it may be useful to monitor renal function.
Elderly patients may have reduced renal function which may not be evident in the results of routine screening tests such as BUN or serum creatinine. A creatinine clearance determination may be more useful. Monitoring of renal function during treatment with gentamicin, as with other aminoglycosides, is particularly important in such patients.
Adverse Reactions
Nephrotoxicity
Adverse renal effects, as demonstrated by the presence of casts, cells, or protein in the urine or by rising BUN, NPN, serum creatinine and oliguria, have been reported. They occur more frequently in patients with a history of renal impairment and in patients treated for longer periods or with larger dosages than recommended.
Neurotoxicity
Serious adverse effects on both vestibular and auditory branches of the eighth cranial nerve have been reported, primarily in patients with renal impairment (especially if hemodialysis is required) and in patients on high doses and/or prolonged therapy. Symptoms include dizziness, vertigo, tinnitus, roaring in the ears and also hearing loss, which, as with the other aminoglycosides, may be irreversible. Hearing loss is usually manifested initially by diminishing high-tone acuity. Other factors which may increase the risk of toxicity include excessive dosage, dehydration and previous exposure to other ototoxic drugs.
Peripheral neuropathy or encephalopathy, including numbness, skin tingling, muscle twitching, convulsions, and a myasthenia gravis-like syndrome, have been reported.
Note: This risk of toxic reactions is low in patients with normal renal function who do not receive gentamicin sulfate at higher doses or for longer periods of time than recommended.
Other reported adverse reactions possibly related to gentamicin include: respiratory depression, lethargy, confusion, depression, visual disturbances, decreased appetite, weight loss, hypotension and hypertension; rash, itching, urticaria, generalized burning, laryngeal edema, anaphylactoid reactions, fever, and headache; nausea, vomiting, increased salivation, and stomatitis; purpura, pseudotumor cerebri, acute organic brain syndrome, pulmonary fibrosis, alopecia, joint pain, transient hepatomegaly, and splenomegaly.
Laboratory abnormalities possibly related to gentamicin include: increased levels of serum transaminase (SGOT, SGPT), serum LDH and bilirubin; decreased serum calcium, magnesium, sodium and potassium; anemia, leukopenia, granulocytopenia, transient agranulocytosis, eosinophilia, increased and decreased reticulocyte counts and thrombocytopenia. While clinical laboratory test abnormalities may be isolated findings, they may also be associated with clinically related signs and symptoms. For example, tetany and muscle weakness may be associated with hypomagnesemia, hypocalcemia, and hypokalemia.
While local tolerance of gentamicin sulfate is generally excellent, there has been an occasional report of pain at the injection site. Subcutaneous atrophy or fat necrosis suggesting local irritation has been reported rarely.
Reactions which may occur because of the solution or the technique of administration include febrile response, infection at the site of injection, venous thrombosis or phlebitis extending from the site of injection, extravasation, and hypervolemia.
If an adverse reaction does occur, discontinue the infusion, evaluate the patient, institute appropriate therapeutic countermeasures, and save the remainder of the fluid for examination if deemed necessary.
Overdosage
In the event of overdosage or toxic reactions, hemodialysis may aid in the removal of gentamicin from the blood, and is especially important if renal function is, or becomes compromised. The rate of removal of gentamicin is considerably lower by peritoneal dialysis than it is by hemodialysis.
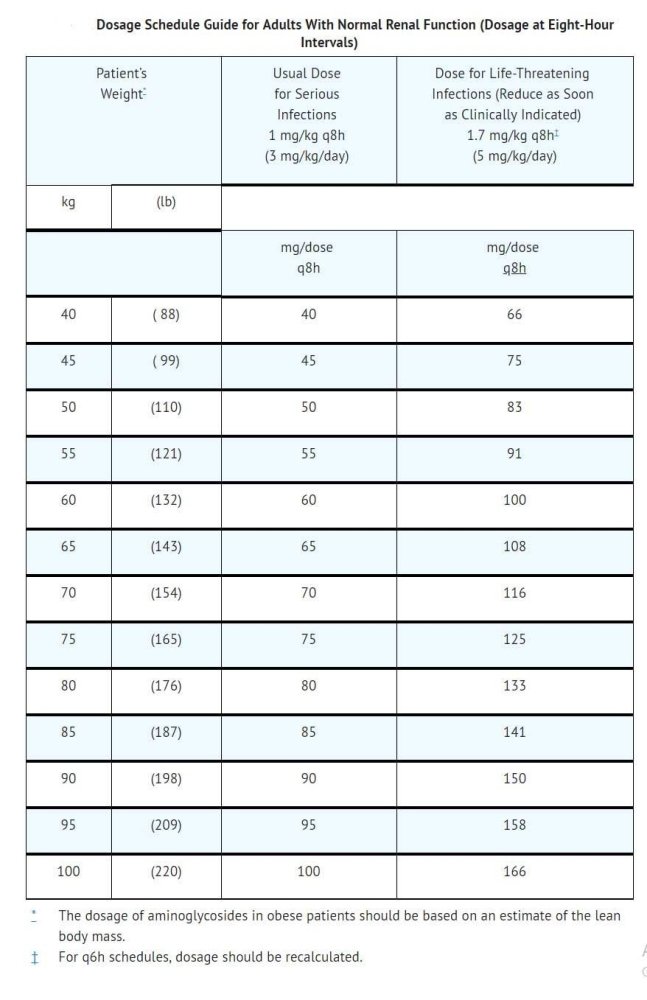
Dosage and Administration
Gentamicin Sulfate in 0.9% Sodium Chloride Injection is for intravenous use only.
The patients pretreatment body weight should be obtained for calculation of correct dosage. The dosage of aminoglycosides in obese patients should be based on an estimate of the lean body mass. It is desirable to limit the duration of treatment with aminoglycosides to short term.
Children: 6 to 7.5 mg/kg/day (2 to 2.5 mg/kg administered every eight hours).
Infants and Neonates: 7.5 mg/kg/day (2.5 mg/kg administered every eight hours).
Premature or Full-Term Neonates One Week of Age or Less: 5 mg/kg/day (2.5 mg/kg administered every 12 hours).
NOTE: For further information concerning the use of gentamicin in infants and children, see Pediatric Gentamicin Sulfate Injection product information.
The usual duration of treatment for all patients is seven to ten days. In difficult and complicated infections, a longer course of therapy may be necessary. In such cases monitoring of renal, auditory, and vestibular functions is recommended, since toxicity is more apt to occur with treatment extended for more than ten days. Dosage should be reduced if clinically indicated.
Directions for Use of VIAFLEX plus Plastic Container
Warning: Do not use plastic containers in series connections. Such use could result in air embolism due to residual air being drawn from the primary container before administration of the fluid from the secondary container is completed.
To Open
Tear overwrap down side at slit and remove solution container. Visually inspect the container. If the outlet port protector is damaged, detached, or not present, discard container as solution path sterility may be impaired. Some opacity of the plastic due to moisture absorption during the sterilization process may be observed. This is normal and does not affect the solution quality or safety. The opacity will diminish gradually. Check for leaks. Do not add supplementary medication.
Preparation for Administration
- Suspend container from eyelet support.
- Remove protector from outlet port at bottom of container.
- Attach administration set. Refer to complete directions accompanying set.
Packing Information